OPD
Allergic Bronchial Asthma
Allergic Bronchial Asthma is recurring episodes of wheezing, chest tightness, coughing, and shortness of breath. This is a chronic inflammatory disorder that is usually triggered by an allergic response to specific allergens, such as dust, mites, pet dander, insect stings, molds, or pollen. A few other things can worsen your condition, including viral respiratory infections, stress, weather conditions, irritants in the air, exercise, and certain food additives.
- Wheezing
- Coughing
- Chest tightness
- Shortness of breath
- Nighttime awakenings due to asthma
- Missed work or school due to asthma
- Requirement for more powerful medications to control symptoms
Medications to control symptoms and prevent attacks, such as:
- Inhaled corticosteroids
- Bronchodilators
- Leukotriene modifiers
- Immunotherapy (allergy shots or sublingual tablets)
Avoidance of allergens and triggers.
Environmental control measures, such as- removing carpets and rugs, using allergen-proof bedding, controlling indoor humidity and avoiding exposure to tobacco smoke and air pollution.
Effective management of allergic bronchial asthma requires a comprehensive approach, includes:
- Working with an allergist to identify and avoid specific allergens
- Using medication as prescribed and adjusting treatment as needed
- Monitoring symptoms and peak flow readings
- Maintaining a healthy lifestyle, including regular exercise and a balanced diet
By understanding the causes, triggers, and treatment options for allergic bronchial asthma, individuals can better manage their symptoms and improve their quality of life.

Pulmonary Hypertension
Pulmonary hypertension refers to increased blood pressure in the arteries that carry blood from the heart to the lungs. This elevated pressure makes it difficult for the heart to function properly and, if left untreated, can lead to heart failure.
- High blood pressure in the lungs, exceeding normal levels
- Increased resistance in the pulmonary arteries
- Blood pressure in the lungs higher than normal
This condition can result from various factors, including lung diseases such as chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis, heart conditions, sleep apnea, blood clots in the lungs, and certain medications.
- Shortness of breath (dyspnea)
- Chest pain or tightness
- Fatigue
- Dizziness or lightheadedness
- Swelling in the legs, ankles, and feet
- Medications to lower blood pressure and improve symptoms
- Oxygen therapy to increase oxygen levels in the blood
- Lifestyle changes, such as quitting smoking and exercising regularly
Interstitial Lung Disease (ILD)
Interstitial Lung Disease, or ILD, is a group of respiratory disorders affecting the interstitium (lung tissue) and the space around the alveoli (air sacs). ILD refers to a group of lung disorders that cause scarring and inflammation in the lungs. This scarring may affect not only the alveolar epithelium but also the pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. As a result of this scarring and inflammation, breathing becomes difficult, and oxygen supply to the bloodstream is compromised. ILD serves as an umbrella term encompassing over 200 conditions classified by histopathological, radiologic, and clinical parameters. Since 2015, approximately 1.9 million people were affected due to this disorder, and 122000 death attributed to ILD in the year.
- Scarring or fibrosis of the lungs, leading to stiffness and difficulty breathing
- Shortness of breath and dry cough
- Other causes include medications, connective tissue diseases, radiation therapy, and inhalation of harmful substances.
Respiratory failure
- Physical therapy
- Supplemental oxygen
- Medications that reduce inflammation or slow the disease progression

Bronchiectasis
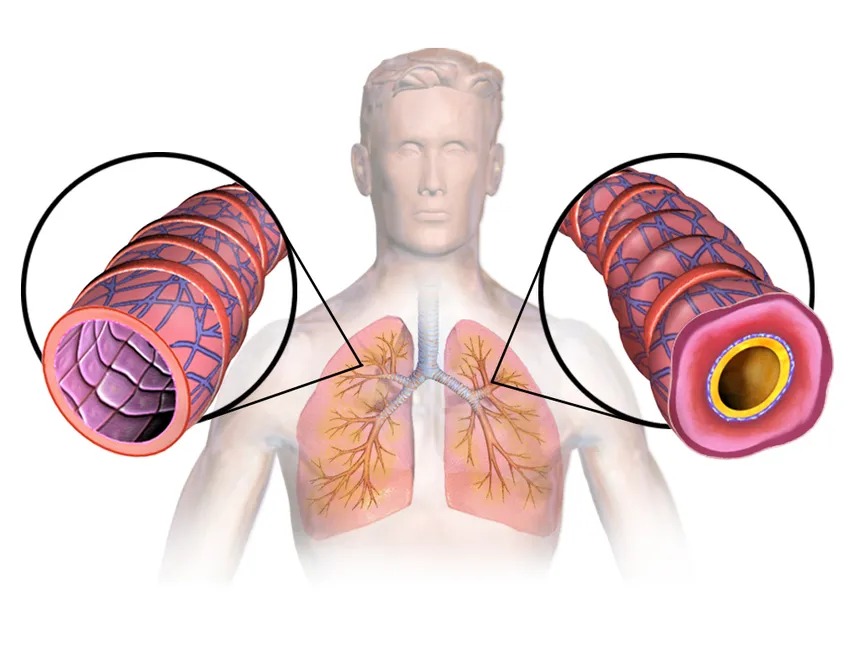
Bronchiectasis is a long-term, chronic lung condition in which the airways become widened, leading to an excess buildup of mucus that makes the lungs more vulnerable to infections. It is often associated with cystic fibrosis. While most people with bronchiectasis can manage the condition and reduce their risk of lung infections, repeated infections can further damage the airways, and there is currently no cure.
The condition may take months or years to develop noticeable signs or symptoms. Once symptoms are diagnosed, the condition may already have worsened. Diagnosis typically involves assessing family history and conducting blood tests to determine any underlying causes of bronchiectasis. Early diagnosis can help prevent extensive lung damage.
Although there is no cure for bronchiectasis, early diagnosis and treatment can help prevent further deterioration of lung function. Patients with bronchiectasis are advised to consult a general practitioner if they develop a persistent cough or to seek help from a specialist for further testing and treatment.
Untreated bronchiectasis can lead to serious complications, such as brain abscesses, collapsed lungs, and heart failure. It is essential to seek medical attention before symptoms worsen or any new symptoms appear.
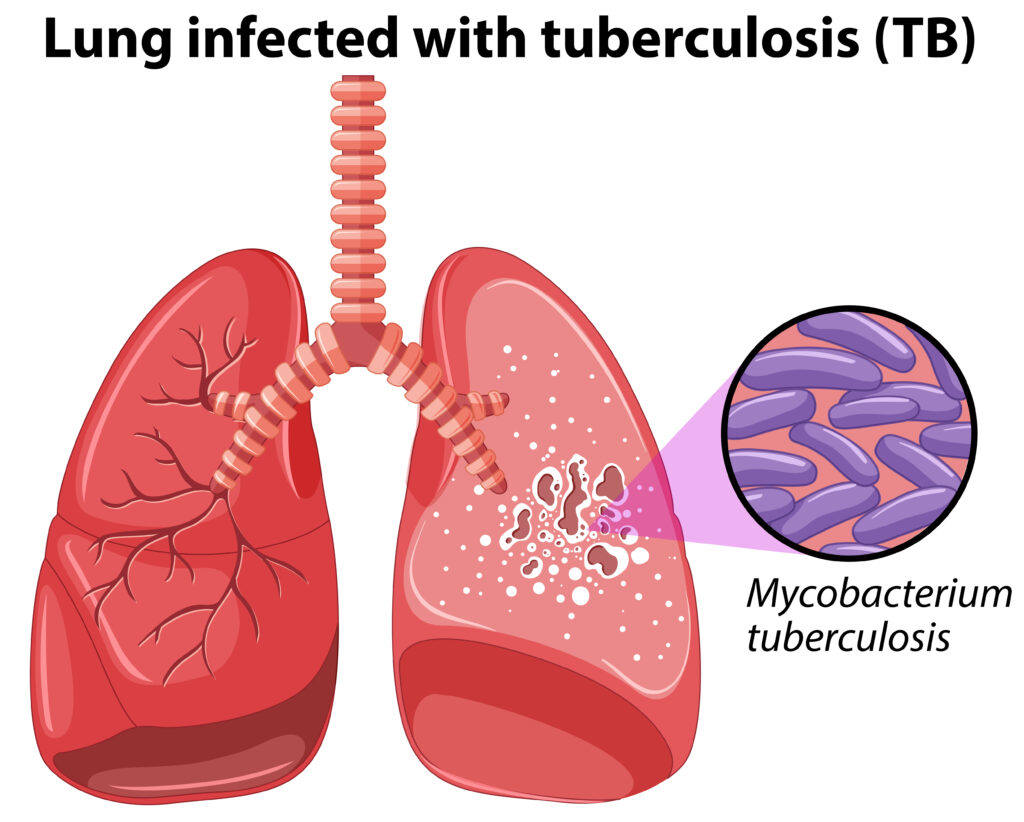
Tuberculosis
Tuberculosis, or TB, also known as “white death,” is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Although this disease can occur with or without symptoms, it primarily attacks the lungs and can slowly spread to other parts of the body. Active TB cases are 50% fatal if untreated.
Before seeking medical help, it is essential to understand the different types of Tuberculosis:
- Pulmonary TB – Affects the lungs
- Extrapulmonary TB – Affects other parts of the body
While TB is caused by Mycobacterium tuberculosis, it spreads through the air when patients with active TB cough, sneeze, or speak. Note that Latent TB has no symptoms and is not contagious, while Active TB is infectious and spreads easily.
Active TB— Fever, Night sweats, Weight loss, Fatigue, and Loss of appetite
Pulmonary TB (Lung-related symptoms)– Chronic cough (often with blood-stained mucus), Chest pain, Shortness of breath, and Coughing up blood (in rare cases)
Extrapulmonary TB (Symptoms vary based on affected organs)–
Symptoms depend on the specific organ involved (e.g., pleura, lymphatic system, central nervous system, or bones).
- Bacteria
The main pathogen is Mycobacterium tuberculosis. This bacterium can survive in dry environments and resist weak disinfectants. - Transmission
An infected person can release up to 40,000 droplets when sneezing. Inhaling even 10 of these droplets can gradually cause TB in a healthy individual.
Certain conditions increase the likelihood of developing TB:
- HIV infection (strongest risk factor)
- Smoking and alcoholism
- Diabetes mellitus
- Malnutrition
- Close contact with an infected person
- Weakened immune systems (due to medications or diseases)
- Vaccination: Bacillus Calmette-Guérin (BCG) vaccine.
- Screening: Regular screening for high-risk groups (e.g., close contacts of TB patients).
- Antibiotics: A combination of multiple antibiotics administered over an extended period.
- Drug Resistance: Growing concern due to multidrug-resistant TB (MDR-TB).
MDR-TB
MDR-TB is a form of tuberculosis that is resistant to at least two first-line anti-TB drugs—rifampicin and isoniazid. This resistance typically occurs due to random mutations that alter the quantity and structure of intracellular drug targets.
- Random mutations in Mycobacterium tuberculosis that alter drug targets.
- Inadequate treatment, poor adherence, and substandard drug quality contribute to the emergence of resistance
- Diagnosis involves molecular testing and culture-based methods.
- Treatment is challenging, often requiring longer regimens with second-line drugs.
- Patients with MDR-TB may experience a poor quality of life due to prolonged treatment and potential side effects
- MDR-TB is a significant public health challenge, particularly in developing countries.
- Efforts to improve TB diagnosis, treatment, and prevention are essential to combat the spread of MDR-TB